Endometriosis is a very frequent condition affecting as much as 10% of reproductive-age women. The condition occurs when endometrium cells begin to grow outside the uterus, usually in the pelvic cavity of the abdomen. Deep endometriosis, one of the most severe forms of the condition, is characterized by the infiltration of organs such as the bladder and the intestine. The inflammation associated with the cyclic detachment of cells from the wrong site during menstruation is responsible for its symptoms, usually pelvic pain, painful menstruation and painful sexual intercourse. Moreover, one of the most bothersome symptoms is the associated infertility.
A review of available evidence on the management of infertility associated with deep endometriosis was conducted by Professor Edgardo Somigliana and Professor Juan Antonio Garcia-Velasco and has been recently published in the Fertility and Sterility journal, under the title “Treatment of infertility associated with deep endometriosis: definition of therapeutic balances“.
The study reviews all published papers in the last 15 years on the subject. Until now, most cases of deep endometriosis with infertility have been managed by surgical treatment, namely using laparoscopic or the so called keyhole surgery. The best estimates of efficacy are based in 40-42% pregnancy rates after surgery, but the evidence is of low quality (case series).
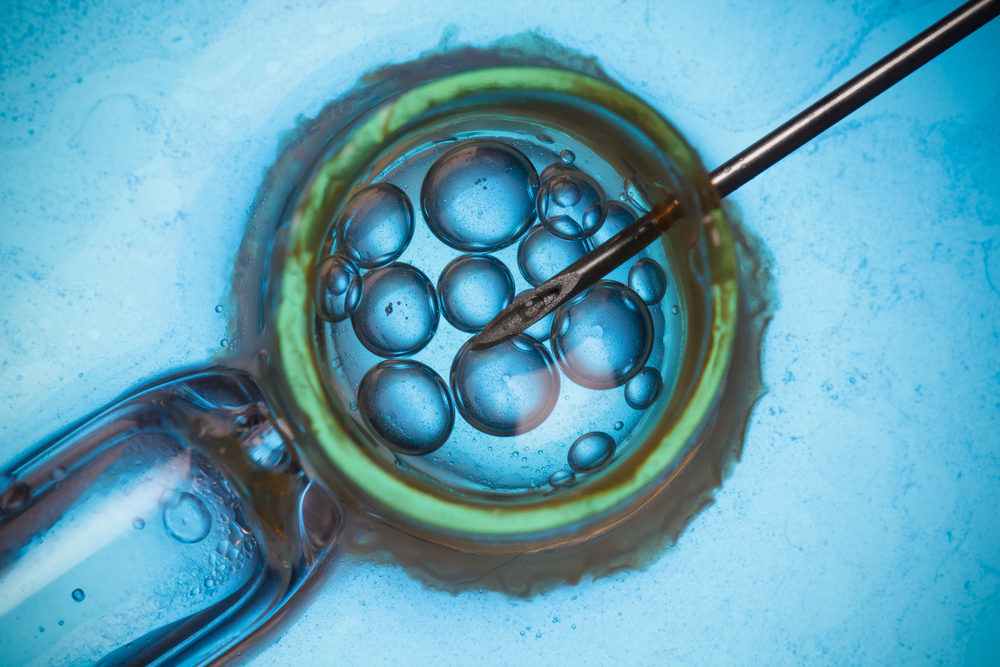
In vitro fertilization (IVF) might be an effective alternative despite the absence of comparative studies. The procedure may be less effective in affected women compared with other indications and it is not without additional deep endometriosis-related risks. Nevertheless, as the causative connection between deep endometriosis and infertility is still not shown, exposing women to surgery and the associated risks with infertility as sole indication is questionable. After reviewing the studies on surgery efficacy, the actual number might be approximately the same as one IVF attempt (25% efficacy).
In the present period of uncertainty, physicians should “first do no harm” and, in the absence of pain symptoms or when they are well controlled under oral medications, IVF should be the first line of treatment. On the other hand, surgery could be necessary in women with concurrent pain symptoms that cannot be effectively managed with oral medications or when those medications are not tolerated or after repeated IVF treatment failures.