A study titled “Uterine Leukocyte Function and Dysfunction: A Hypothesis on the Impact of Endometriosis” explored the impact of leukocytes in the uterus and their role in endometriosis. The study, published in the journal American Journal of Reproductive Immunology, may help uncover potential new treatments for the disease.
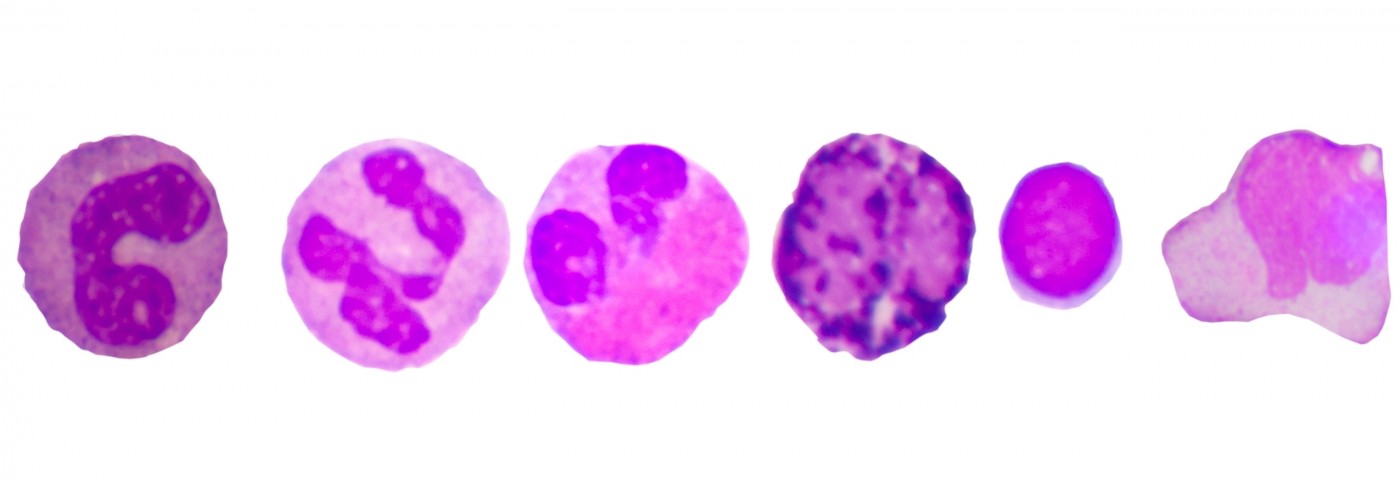
Previous studies have reported alterations in a population of immune cells called leukocytes (white blood cells that help fight off disease) within the ectopic and eutopic tissue of the endometrium. Now, Michigan State University researchers reviewed the difference between two types of immune cells, the uterine natural killer cells (NK cells are the predominant leukocyte population in the normal human endometrium) and regulatory T cells within the eutopic endometrium between patients with endometriosis and healthy controls.
They focused on how differences in these two cell types associate with failure for implantation and in the clearance of the endometrium during the menstrual cycle. Although some studies found that deregulation of uterine NK cells number or function could lead to implantation failure in patients with endometriosis (and suggest that differences in these cells may turn the uterus microenvironment less receptive to embryo implantation), other studies found no differences.
Researchers emphasize that additional studies are required to fully understand how changes in uterine NK cells may increase the risk of implantation failure in these patients.
The population of regulatory T cells (often identified by expression of the transcription factor forkhead box P3, FoxP3) secretes immunosuppressive cytokines, inducing a state of immune tolerance. This phenomenon is thought to be required for a successful embryo implantation. Infertile patients often exhibit lower levels of Foxp3 mRNA when compared to fertile patients.
In endometriosis, studies in both a baboon model with endometriosis and human patients suggest that endometriosis changes the levels of regulatory T cells in the endometrium. morestudies are necessary to assess the number and function of uterine regulatory T cells in more patients with endometriosis. Moreover, there is a lack of information on the role of regulatory T cells in menstruation and how that affects the shedding of endometrial tissue.
In fact, the team hypothesized that if uterine regulatory T cell functions are altered in endometriotic lesions, they may promote survival of endometrium, contributing to the progression of the disease.
The authors note that additional studies should address the role of these immune cells in endometriosis, possibly identifying novel targets for future therapies.