Endometrial stromal fibroblasts are crucial for the cyclic regeneration of the endometrium. A recent study showed that endometrial mesenchymal stem cells are the forebearers of such fibroblasts, already harboring the defective progesterone sensitivity that typifies the disease.
A commentary to the study, “Human endometrial fibroblasts derived from mesenchymal progenitors inherit progesterone resistance and acquire an inflammatory phenotype in the endometrial niche in endometriosis,” highlights that such milestone findings demand further research, aiming to elucidate the mechanisms of the disease.
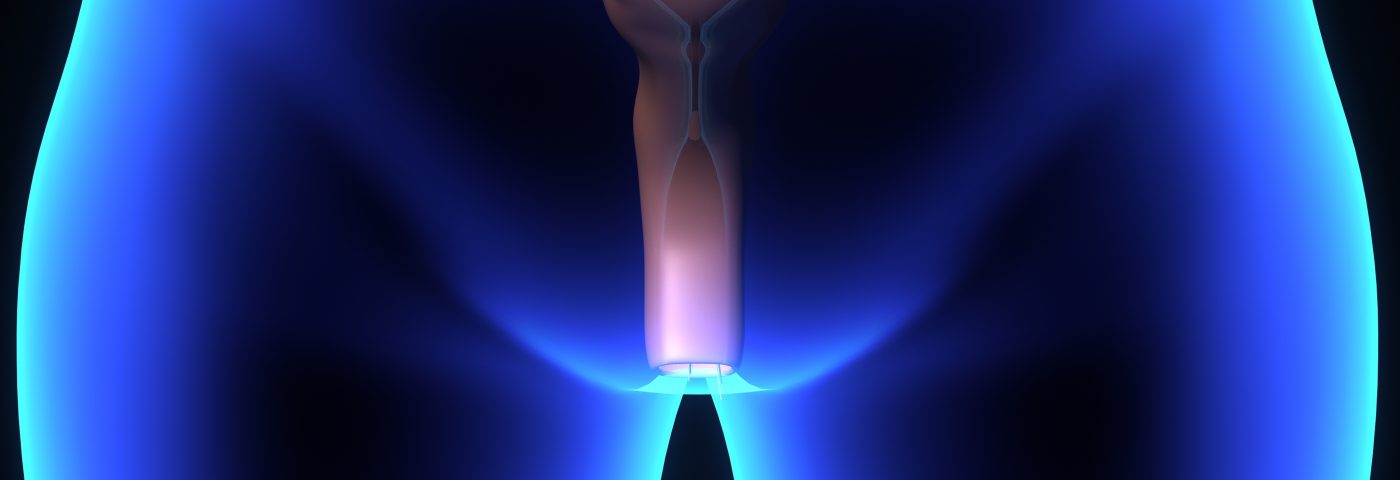
Endometrial stromal fibroblasts are a cell type crucial for the normal functions of the endometrium, and are usually highly responsive to the hormone progesterone. In this process, called decidualization, the cells are involved in establishing pregnancy or, in the absence of pregnancy, for the shedding of tissue during menstruation — functions that are disrupted in endometriosis.
These fibroblasts also have profound inflammatory characteristics, a feature indicating that the cells likely contribute to endometriosis and associated infertility.
Endometrial mesenchymal stem cells are equally good candidates for playing a role in the disease, but despite much research, the role of these stem cells in endometrial health and disease is not clear. Here, University of California, San Francisco, researchers used gene profiling, bioinformatics, and in vitro studies to show that defective progesterone responses — or progesterone insensitivity— in endometriosis originate in these mesenchymal stem cells.
Comparing newly isolated endometrial cells with cells cultured for brief and for prolonged periods of time, the researchers also revealed that the defect is not genetic. Moreover, they showed that the pro-inflammatory characteristics of endometrial stromal fibroblasts are not passed on from its stem cell precursors, painting a rather complex picture of the molecular changes accompanying endometriosis.
A commentary to the study, titled “Endometrial mesenchymal stem/stromal cells, their fibroblast progeny in endometriosis, and more,“ and published in the same journal — Biology of Reproduction — underscored the importance of the findings, calling them a “major contribution” to the field of mesenchymal stem cells.
Researchers from the Hudson Institute of Medical Research, Australia, who authored the commentary, wrote it is now crucial to find out what mechanisms lead to the defect in the stem cells from the start. More studies are needed, they said, to determine if epigenetic changes or microRNA gene regulation might contribute.
Identifying the factors responsible for triggering the inflammatory characteristics of the fibroblasts is also crucial, as is the evaluation of the role of mesenchymal stem cells in causing disease by retrograde menstruation.
Most importantly, the commentary said that an exploration of drug-based approaches to promote the development of endometrial stromal fibroblasts that have restored decidualization characteristics are among the efforts needed now.